Chronic Liver disease is a term that covers a broad range of conditions affecting one of the most critical organs in your body: the liver. This organ isn’t just a passive participant in your body’s functioning. It is a powerhouse that plays a central role in your metabolism, energy storage, and detoxification processes.
In simple terms, your liver helps you digest your food, convert it into energy, and store that energy until your body needs it. It’s also your body’s main filter, removing harmful substances from your bloodstream. According to John Hopkins Medicine, the liver has over 500 vital functions. Considering all the roles played by the liver, any impairment to its function can have significant consequences.
Therefore, the terminology liver disease represents a group of conditions that can affect the liver in different ways. When health experts call it liver disease, they’re usually referring to chronic conditions that do progressive damage to your liver over time. Some of these conditions are relatively common, while others are more rare. Understanding liver diseases—their causes, symptoms, and treatments—can help you better appreciate how to protect this vital organ and what to do if something goes wrong.
The Four Stages of Chronic Liver Disease

Chronic liver disease is a serious and progressive condition that gradually impairs liver function over time. The disease unfolds in four distinct stages:
- Hepatitis
- Fibrosis
- Cirrhosis
- Liver Failure.
Understanding these stages is crucial for early detection, effective management, and potentially slowing the progression of the disease.
Stage 1: Hepatitis – The Initial Inflammation
The first stage of chronic liver disease is hepatitis, which refers to inflammation in the liver tissues. Inflammation is the liver’s natural response to injury or the presence of toxins. Ideally, inflammation is a protective mechanism aimed at eliminating infections and initiating the healing process. Acute hepatitis, a condition characterized by a temporary and immediate inflammatory response, can often resolve the issue if the cause of injury is addressed promptly.
However, when the source of damage persists as a result of chronic alcohol consumption, viral infections like hepatitis B or C, or ongoing exposure to toxins, the inflammation becomes chronic. In chronic hepatitis, the liver’s healing processes become overactive, leading to excessive tissue repair. This ongoing inflammation and repair cycle eventually results in the formation of scar tissue, marking the transition to the next stage of liver disease: fibrosis.
Stage 2: Fibrosis – The Accumulation of Scar Tissue
Fibrosis is the second stage of chronic liver disease. Fibrosis involves the gradual accumulation of scar tissue in the liver. As inflammation continues from the hepatitis stage, the liver attempts to repair itself, but this process often results in the formation of fibrous scar tissue. This scar tissue forms thin bands throughout the liver, gradually stiffening the organ.
The accumulation of scar tissue disrupts normal liver function by restricting blood flow through the liver. When a reduction of blood flow occurs, the liver receives less oxygen and fewer nutrients, which are essential for its vitality and function. Over time, this leads to a gradual decline in the liver’s overall health and ability to perform its vital roles in the body.
Despite the seriousness of fibrosis, it is important to note that some levels of fibrosis are reversible. If the underlying cause of liver damage is addressed and slowed down, the liver’s remarkable regenerative abilities can come into play. Healthy liver cells can regenerate, and some of the scar tissue may diminish, potentially restoring some liver function.
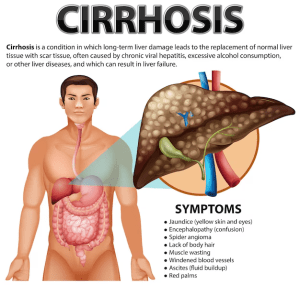
Stage 3: Cirrhosis – Irreversible Scarring
Cirrhosis represents the third stage of chronic liver disease. This stage is characterized by severe, permanent scarring of the liver. At this point, the fibrosis that began in the earlier stages has progressed to the extent that the liver is significantly compromised. Unlike fibrosis, where some scarring is reversible, cirrhosis damage is irreversible.
Having cirrhosis means that the liver has lost a substantial number of healthy cells, which are essential for its regenerative capacity. The remaining liver tissue is heavily scarred and can no longer regenerate effectively. As a result, liver function begins to decline. Although the liver is still working, its reduced capacity means that it can no longer perform all of its functions efficiently.
During this stage, the effects of liver damage may start to become more evident. However, the body has an incredible ability to compensate for liver dysfunction, often masking the symptoms of cirrhosis in the early stages. This compensation can delay the onset of noticeable symptoms, sometimes giving a false sense of security. Nevertheless, the damage continues to progress, and without intervention, cirrhosis inevitably leads to the final stage: liver failure.
Stage 4: Liver Failure – The End Stage
In this stage, the liver can no longer function adequately to meet the body’s needs. This stage is also referred to as “decompensated cirrhosis” because the body’s ability to compensate for the loss of liver function is exhausted.
As liver functions begin to break down, the effects are felt throughout the body. Symptoms of liver failure are often severe and can include jaundice (yellowing of the skin and eyes), severe fatigue, confusion, swelling in the legs and abdomen (edema and ascites), and bleeding disorders due to the liver’s inability to produce essential clotting factors.
Chronic liver failure is a gradual process, but it is ultimately fatal without a liver transplant. The liver is a vital organ with functions that are critical to life, including detoxifying the blood, producing bile for digestion, and regulating metabolism. Once the liver fails, the body’s ability to perform these essential functions is lost, leading to life-threatening complications.
What Are the Common Signs and Symptoms of Chronic Liver Disease?
Once the liver is impaired, the body experiences many symptoms which vary depending on the specific condition. In some people, disease of the liver can go unnoticed for years because the symptoms are either mild or non-existent in the early stages. However, as the liver is severely damaged, symptoms do occur. These may include:
Jaundice
This is one of the most recognizable symptoms of liver disease. This happens when the liver’s ability to process and excrete bilirubin, a yellow pigment produced from the breakdown of red blood cells. Also, this can result from the presence of other conditions such as hepatitis or cirrhosis. These conditions may damage the liver cells or obstruct the bile ducts. This makes bilirubin accumulate in the blood because it cannot be efficiently processed or excreted. The result of this buildup is the yellowing of the skin and eyes, characteristic of jaundice.
Changes in stool colour
Liver disease can cause changes in stool colour primarily due to its impact on bile production and flow. When the liver is damaged, it may produce less bile. This bile flow may be obstructed by conditions like cirrhosis or bile duct stones. Since bile is responsible for the brown colour of stool, reduced bile quantity results in pale or clay-coloured stools. Conversely, if there is bleeding in the upper gastrointestinal tract, stools may appear black. Also, if there is increased bile in the intestines, stools might become unusually dark or even green.
Ascites
Ascites is the accumulation of fluid in the abdominal cavity, often caused by liver disease, particularly cirrhosis. Damage to the liver causes increased pressure in the veins of the liver (portal hypertension). This also disrupts the balance of fluids in the body. This pressure causes fluid to leak from the blood vessels into the abdominal cavity (ascites). This causes other signs and symptoms such as abdominal swelling, discomfort, and a noticeable increase in abdominal girth. It may also be accompanied by other symptoms such as difficulty breathing and an increased risk of infections.
Hepatic encephalopathy
This is a condition where toxins build up in the brain due to liver dysfunction. It occurs when the liver fails to filter or excrete toxins such as ammonia effectively from the blood. This ammonia accumulates in the blood and crosses the brain-blood barrier. Elevated ammonia levels in the brain disrupt neurotransmitter function and neuronal activity, leading to cognitive dysfunction, confusion, and altered mental status. This also leads to mood changes, sleep disturbances, and cognitive impairment. Here are more signs related to complications of chronic liver disease: https://shorturl.at/9tQ6m
What Are Common Causes of Liver Disease?
Several liver diseases are relatively well-known, and each has its causes, symptoms, and treatment options. Here are some of the main ones:
1. Hepatitis
Hepatitis is an inflammation of the liver. When it is caused by a virus, it’s called viral hepatitis. Currently, there are five known types of this viral infection, including Hepatitis A, B, C, D, and E. An individual contracts Hepatitis A and E through contaminated food or water. These types resolve on their own, though recovery can take weeks. Hepatitis B, C, and D, however, are more serious and can lead to chronic liver damage. Hepatitis B and C are particularly concerning because they can lead to chronic liver disease, cirrhosis, or liver cancer if not properly managed. Hepatitis B is spread through bodily fluids like blood and semen, while Hepatitis C is often contracted through blood contact, such as through shared needles.
2. Fatty Liver Disease
As the name suggests, fatty liver disease is characterized by a buildup of fat in the liver. There are two main types of this condition;
Alcoholic fatty liver disease. This is caused by excessive alcohol consumption.
Nonalcoholic fatty liver disease (NAFLD). This is not related to alcohol use. It is often associated with obesity and metabolic syndrome. If left unchecked, fatty liver disease can progress to more serious conditions like cirrhosis and liver failure.
3. Autoimmune Conditions
Some liver diseases are caused by the body’s immune system mistakenly attacking its liver cells. For example, autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis are all caused by the malfunctioning of the immune system. Autoimmune hepatitis when not treated on time leads to liver inflammation, cirrhosis, and liver failure. PBC damages the bile ducts within the liver, leading to a buildup of bile, which in turn causes liver damage. Primary sclerosing cholangitis similarly affects the bile ducts, leading to blockages and subsequent liver damage.
4. Genetic Conditions
Certain liver diseases run in some families and are hereditary. Hemochromatosis, for example, is one condition that causes the body to store too much iron. This iron accumulates in the liver and other organs, causing damage. Wilson’s disease is another example of a liver problem caused by faulty genes. It leads to the buildup of copper in the liver, which can also damage the brain and other organs. Additionally, the Alpha-1 antitrypsin deficiency condition also affects the liver’s ability to produce a protein that protects against enzyme damage, leading to liver and lung disease.
5. Drug-Induced Liver Disease
Once you take drugs or supplements, the liver metabolizes them through chemical processes to make them easier to excrete. It first modifies the drugs (Phase I) using enzymes, then further transforms them into water-soluble forms (Phase II) to facilitate their elimination from the body via bile or urine. However, taking some drugs over a long time or in excessive dosage may damage the liver, causing drug-induced liver disease. This damage disrupts liver function, leading to symptoms like jaundice, abdominal pain, and altered mental status, and potentially resulting in serious conditions like liver failure.
6. Liver Cancer
Cancer of the liver occurs as a complication of having one or multiple liver problems. It often develops as a secondary condition when other liver diseases, particularly cirrhosis, go untreated. One most common types of liver cancer is hepatocellular carcinoma which presents as multiple small tumors within the liver.
7. Cirrhosis
Cirrhosis is a medical condition that occurs when there is scarring of the liver. Many factors can cause this scarring, including long-term damage from various liver diseases as a result of alcohol use and hepatitis. Ideally, the liver can regenerate even after damage. However, this regeneration often results in scar tissue, which hinders the liver’s ability to function. Advanced cirrhosis leads to liver failure, a condition where the liver can no longer perform its essential tasks.
What Are the Risk Factors for Liver Disease?
Having certain behaviours and conditions may increase your risk of developing liver disease. One of the most well-known risk factors is heavy alcohol consumption. According to the Centers for Disease Control and Prevention (CDC), heavy drinking is defined as having more than 8 drinks per week for women. For men drinking more than 15 drinks per week. Other risk factors include:
- I am sharing sharp objects such as razors and needles.
- Getting tattoos or body piercings with non-sterile needles.
- Occupational exposure to blood and other bodily fluids
- Having unprotected sex
- Living with conditions like diabetes or high cholesterol
- Having a family history of liver disease or any other genetic material that exposes you to liver problems.
- Carrying excess weight
- Exposure to environmental toxins like pesticides
- Taking certain medications or supplements in large amounts can damage the liver.
How to Prevent Liver Disease
While not all liver diseases can be prevented, healthy lifestyle choices can significantly reduce your risk. For instance, maintaining a nutritious diet, staying physically active, limiting alcohol intake and avoiding drugs that damage the liver may keep your liver cells healthy and functional. Also, avoiding smoking is another key strategy you can take to protect your liver. The American Liver Foundation advises people to be cautious with chemicals, practise safe sex, and get regular check-ups that include blood work to monitor liver health. Here are more tips on how to prevent liver disease: https://shorturl.at/hXgls
How is Chronic Liver Disease Diagnosed?
If you suspect you might have liver disease, it’s important to see a healthcare professional. Diagnosis typically begins with a review of your medical history and an assessment of your symptoms. Your doctor might ask about your alcohol consumption, diet, and any medications or supplements you’re taking. From there, they may recommend liver function tests, imaging tests like CT scans or MRIs, or a liver biopsy to determine the extent of liver damage.
Treating Chronic Liver Disease
Treatment for liver disease depends on the specific condition, but many liver diseases are chronic and require long-term management. Lifestyle changes like reducing alcohol intake, maintaining a healthy weight, and eating a liver-friendly diet are often crucial. Medical treatments might include antiviral medications for hepatitis, steroids to reduce inflammation, and various drugs to manage symptoms or prevent complications. In severe cases, surgery or a liver transplant might be necessary. Here are more ways of treating each disease in chronic liver disease: https://www.ncbi.nlm.nih.gov/books/NBK554597/