Image from:https://shorturl.at/ahKAs
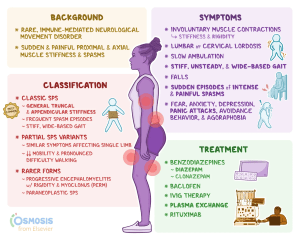
Stiff Person Syndrome (SPS) is a rare autoimmune disorder that primarily affects the central nervous system. It is a complex autoimmune neurological disorder characterized by severe muscle stiffness and painful spasms.
With time, these spasms lead to significant discomfort and disability. Unlike typical muscle cramps, the stiffness in SPS is more persistent, affecting the posture and gait in people. If not treated, Stiff Person Syndrome causes an exaggerated curve in the lower back (hyperlordosis) and difficulty walking.
In most people, SPS is diagnosed when these individuals are in their 40s and 50s. SPS affects women more than men and affects one to two people per million. Health experts from the National Institute of Neurological Disorders and Stroke (NINDS) report that SPS may be underdiagnosed, suggesting that the true prevalence could be higher. This article analyses the SPS, exploring its manifestations, diagnostic criteria, treatment options, and the latest research in the field.
What Are the Causes and Pathophysiology of Stiff Person Syndrome?
Ideally, the cause of Stiff Person Syndrome remains unknown. However, medical experts and researchers argue that SPS could be caused by an autoimmune reaction. How does this occur? The human body produces many neurotransmitters, which are chemical messengers in the brain. One such chemical messenger is gamma-aminobutyric acid (GABA). GABA is produced by a protein called glutamic acid decarboxylase (GAD). The immune system mistakes GAD for pathogens and attacks it, causing low levels of GABA production.
GABA is a key neurotransmitter and is responsible for regulating motor neurons by decreasing their activity. Having low GABA levels causes the brain neurons to fire continuously even when they’re not supposed to. This results in all the signs and symptoms we see in people suffering from Stiff Person Syndrome. Scientists link autoimmunity to SPS condition because anti-GAD antibodies are found in 60-80 per cent of patients with Stiff Person Syndrome. These anti-GAD antibodies are either identified in their blood or the cerebrospinal fluid (a water-like substance surrounding the brain).
The disease is also linked to other chronic illnesses. For instance, most people suffering from SPS have other conditions as well which are linked to autoimmunity. These conditions may include type 1 diabetes, vitiligo, and pernicious anemia. Stiff Person Syndrome seems to be prevalent in people having specific types of cancer. Scientists have found that SPS is most present in people with breast cancer, lung cancer, kidney cancer, thyroid cancer, colon cancer, and lymphoma. The studies are still ongoing to establish the exact cause of this link and find its causing factors. Understand more causes of SPS here: https://shorturl.at/McyK9
What Are the Symptoms of Stiff Person Syndrome?

Image from:https://shorturl.at/FCswA
Muscle Stiffness and Spasms.
These are the most prominent symptoms of SPS. This severe stiffness primarily affects the trunk and limbs and gets worse as SPS progresses. Any sudden movement, stress, or even environmental factors such as cold temperatures may trigger the painful spasms.
Difficulty Walking.
Persistent muscle stiffness, cramps and spasms makes an individual to develop an abnormal gait. This makes it difficult to maintain body balance, making individuals with SPS walk with a wide stance and may fall.
Postural Abnormalities.
As the disease goes into its advanced stages, it changes the posture of a person. One of the most common postural abnormalities in SPS is hyperlordosis, where the lower back curves inward. This abnormality causes severe pain and discomfort in individuals.
Breathing Difficulties.
In its advanced stages, SPS spasms may affect the muscles of the chest and throat. This leads to shortness of breath and respiratory issues, including death.
Psychological Impact.
People living with SPS live in fear of sudden spasms, which often lead to anxiety and agoraphobia. Many patients become increasingly isolated, fearing that a sudden spasm could occur in public or during a stressful situation. Here are the conditions with similar symptoms to SPS: https://shorturl.at/N6jGr
What Are the Types of Stiff Person Syndrome?
Each SPS type presents unique symptoms and challenges, making it difficult to understand the condition fully. Types include:
Classic Stiff Person Syndrome
This is the most common form of SPS. It is characterized by muscle stiffness and spasms primarily in the lower back, legs, and occasionally the abdomen. People with classic SPS often report experiencing frequent spasms and chronic pain, which makes it difficult for them to perform daily activities.
Partial Stiff Person Syndrome
This type of SPS is also known as Stiff Limb Syndrome, Stiff Leg Syndrome or Stiff Trunk Syndrome. It is not so common, and the muscle spams are usually localized to a specific area, usually one leg. In its severe cases, the stiffness may attack the trunk or abdomen, but it remains limited compared to classic SPS.
Stiff Person Syndrome Plus
This is a very rare SPS type and is a more complex form of the disorder. It presents with symptoms of classic SPS and additional neurological symptoms such as double vision, lack of coordination, and slurred speech. Scientists argue that these neurological symptoms are caused by dysfunction in the brainstem and cerebellum. This is what makes this type more challenging to diagnose and manage.
Other Less Common Variants
Other variants of SPS recognized by health experts are:
Progressive Encephalomyelitis with Rigidity and Myoclonus (PERM).
This one is characterised by many neurological symptoms.
Predominant/Pure Cerebellar Ataxia.
This primarily involves coordination and balance issues due to cerebellar dysfunction without significant muscle rigidity.
Overlapping syndrome.
This form of SPS is a combination of classic SPS symptoms (muscle stiffness and spasms) with additional features from other neurological conditions, such as cerebellar ataxia or brainstem dysfunction.
Diagnosis of Stiff Person Syndrome
SPS is a rare and complex condition, making it difficult to diagnose and treat. Its rare existence means it is less studied, highly misdiagnosed or underdiagnosed, hence poor treatment outcomes. Diagnosing SPS requires systematic clinical observations, thorough patient history and specific diagnostic tests such as:
Blood Tests. Blood tests are the most basic test in diagnosing SPS. Blood tests are essential as they help in detecting anti-GAD65 antibodies. 80% of people with a positive test of SPS have elevated levels of these antibodies. Blood tests can also be used to screen for other antibodies, such as anti-amphiphysin and anti-glycine receptors, which are associated with SPS variants.
Electromyography (EMG). This test is used to analyse the electrical activity of muscles. If the test detects the presence of continuous muscle activity, the diagnosis of SPS is confirmed. This is because continuous muscle activity is a hallmark of SPS. Before patients are given this test, they are usually advised to halt all activities that may trigger muscle shakiness.
Lumbar Puncture. This procedure is also called a spinal tap. It is performed by inserting a long sterile needle into the lower back, in between the lumbar vertebrae. It collects the cerebrospinal fluid, which is then analysed for the presence of anti-GAD65 antibodies and to rule out other conditions.
Imaging Studies. MRI and CT scans are often used to rule out other neurological disorders that may present with similar symptoms. In cases of paraneoplastic SPS, FDG-PET scans may be utilized to detect underlying cancers.
Treatment Options for Stiff Person Syndrome
Unfortunately, the Stiff Person Syndrome has no cure. Health experts focus on the management of symptoms to alleviate pain and prolong life. Its management involves a combination of medications, therapies, and lifestyle modifications to help manage symptoms to improve the quality of life.
Medications to Manage Symptoms
Muscle Relaxants. These are the most common medications prescribed to manage the SPS symptoms. They include diazepam, clonazepam, baclofen, and tizanidine. These medications work on the central nervous system and help reduce muscle stiffness and alleviate spasms. This creates mobility and comfort in patients.
GABAergic Medications. These are medications such as gabapentin, pregabalin, and tiagabine. They work by enhancing the effects of GABA in the brain, hence reducing the excessive firing of neurons.
Botulinum Toxin. In some types of SPS where the muscle spasms are localized, botulinum toxin injections may be used. This works by temporarily paralyzing specific muscles to reduce localized muscle spasms and stiffness. With time, this improves mobility and comfort in affected areas.
Immune-Based Therapies
SPS is an autoimmune disorder, and therefore some of its treatments are aimed at targeting the immune system. They include:
Intravenous Immunoglobulin (IVIG). This is one of the best immune-based therapies for SPS. Here, healthy individuals donate antibodies which are then administered to individuals with SPS. This helps in modulating the immune response, stopping it from attacking healthy body cells and tissues. This treatment has been shown to reduce stiffness and improve mobility in SPS patients.
Plasma Exchange or Plasmapheresis. This is another key procedure that removes the patient’s blood plasma and replaces it with donor plasma. Doing this reduces the levels of harmful antibodies in the bloodstream.
Immunosuppressants. These medications include rituximab, mycophenolate mofetil, and azathioprine. They work by suppressing the immune system to prevent further attacks on the nervous system.
Non-Medication Therapies
SPS management does not solely rely on medications only. Because of the complex nature of SPS, adopting various non-pharmacological therapies can help manage the symptoms effectively. They include:
Physical Therapy. Physical therapy plays a crucial role in maintaining mobility and preventing the worsening of symptoms. Therapists may focus on stretching exercises, deep tissue myofascial techniques, and balance training.
Aquatic Therapy. Water-based exercises in warm pools can help relax muscles and improve mobility without putting excessive strain on the body.
Alternative Therapies. As more treatment modalities are being discovered, scientists are advocating for techniques such as acupuncture and chiropractic care. The techniques are key in providing relief to some SPS patients. Other techniques may include massage therapy and yoga. These therapies may not create comfort in every patient, but they can be valuable additions to a comprehensive treatment plan. Here are more treatment options: https://shorturl.at/M9NXU
Lifestyle Modifications and Coping Strategies for SPS
Living with Stiff Person Syndrome (SPS) involves adopting various lifestyle modifications and coping strategies. These modifications are crucial in managing symptoms effectively and improving overall quality of life. Here are some coping strategies you can adopt:
Regular Exercise and Physical Activity
Engaging in regular, gentle exercise can help maintain mobility and flexibility. Adopt activities such as stretching, swimming, and walking which can be beneficial to your muscles and body. It’s important to work with a physical therapist to develop a personalized exercise plan that accommodates your condition. If your condition is not that serious, focus on exercises that help prevent muscle stiffness and spasms.
Stress Management
Stress is a factor known to exacerbate SPS symptoms. Therefore, it is important to find effective stress management techniques. Practices such as mindfulness meditation, deep breathing exercises, and relaxation techniques can help reduce stress and improve emotional well-being. You can also go for Cognitive Behavioral Therapy (CBT), which is ideal for managing anxiety and improving coping strategies.
Ergonomic Adjustments
Making ergonomic adjustments to your living and working spaces can help reduce muscle strain and discomfort. Ensure that your workspace is set up to support good posture. Use supportive furniture and assistive devices if needed.
Warmth and Comfort
Cold causes severe muscle cramps and stiffness. Therefore, keeping warm can help prevent muscle spasms in winter or when in cold environments. Using heating pads, warm baths, and dressing in layers can help maintain body warmth and reduce muscle stiffness.
Dietary Considerations
While there is no specific diet for SPS, maintaining a balanced diet is important in supporting overall health and well-being. Also, staying hydrated, and consuming adequate vitamins and minerals will improve your general health. Avoiding excessive caffeine and alcohol can help in keeping your body in check. If you have any dietary restrictions or specific health concerns, consult a nutritionist.
Support Networks
Building a support network of family, friends, and support groups can provide emotional support and practical assistance. Connecting with others who have SPS or similar conditions can offer valuable insights and encouragement.
Regular Medical Follow-ups
Regular follow-up visits with healthcare providers are essential to monitor the progression of the condition and adjust treatment plans as needed. Keeping an open line of communication with your healthcare team can help ensure that your treatment plan remains effective and up-to-date.
Frequently Asked Questions (FAQs).
Q1. Is there a cure for Stiff Person Syndrome?
Currently, there is no cure for SPS. However, treatment options are available to help manage symptoms and improve quality of life. Medications, immune therapies, and non-medication treatments can help reduce muscle stiffness, spasms, and pain.
Q2. What are the early signs of Stiff Person Syndrome (SPS)?
Early signs of SPS often include muscle stiffness and spasms that may start in the legs and back. Other initial symptoms may include difficulty walking, an unsteady gait, and a rigid posture. Some individuals may experience muscle cramps or stiffness in specific areas before other symptoms develop.
Q3. What is the Life Expectancy for Stiff Person Syndrome?
The life expectancy for individuals with Stiff Person Syndrome (SPS) can vary widely and is generally not significantly reduced compared to the general population. However, severe symptoms and complications may impact quality of life. Effective management and treatment can help improve life expectancy and overall well-being.
Q4. What Triggers Stiff Person Syndrome?
Stiff Person Syndrome can be triggered by factors such as stress, sudden movements, cold temperatures, and certain physical activities. Emotional stress and unexpected stimuli are particularly known to exacerbate muscle spasms and stiffness.
Q5. Is Stiff Person Syndrome Painful?
Yes, Stiff Person Syndrome can be painful. The condition often causes muscle stiffness and spasms, which can lead to chronic pain and discomfort, particularly in affected muscles and joints.